A Common Question With an Important Answer
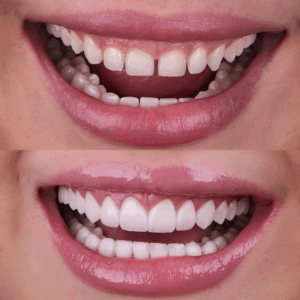
When you lose a tooth, the gap left behind affects more than just your smile. It changes how you chew, speak, and feel about yourself. Naturally, many people look for a permanent fix, and dental implants are widely considered the gold standard for tooth replacement. However, for patients who smoke, the path to a restored smile often comes with extra questions and concerns.
You might have heard rumors that smoking automatically disqualifies you from getting implants, or perhaps you worry that your history with tobacco will cause the procedure to fail. These are valid concerns. Smoking affects oral health in significant ways, altering how gums heal and how bone regenerates.
We’ll clarify specific risks involved, explain why nicotine changes the healing process, and outline what dentists recommend to help you get the best possible result.
How Dental Implants Work
Unlike a denture that rests on top of the gums or a bridge that relies on neighboring teeth, an implant replaces the entire tooth structure, from root to crown.
- The Post: This is a small screw, usually made of titanium or zirconia. It serves as the new root for your tooth.
- The Abutment: This connector piece sits on top of the post and holds the restoration in place.
- The Crown: This is the visible part of the tooth, custom-made to match your natural smile.
The Importance of Osseointegration
Dental Implants involve a biological process called osseointegration. After the surgeon places the titanium post into the jaw, the bone must grow around it and fuse to the metal surface. This fusion provides the stability needed to chew tough foods without the tooth moving. Because this process relies entirely on the body’s natural ability to repair itself, anything that slows down or stops healing becomes a major concern.
How Smoking Affects Dental Implant Success
Reduced Blood Flow to the Gums
Nicotine is a vasoconstrictor. This means it causes the tiny blood vessels in your gums and jawbone to shrink. Blood carries oxygen, nutrients, and immune cells to the site of a wound to help it heal. When you smoke, you restrict this supply line. The result is slower healing and a higher risk that the gum tissue around the implant will not close properly.
Higher Chance of Implant Failure
Clinical observations show that smokers face a higher rate of implant failure compared to non-smokers. If the bone does not receive enough blood flow, it may fail to fuse with the titanium post. If osseointegration does not happen, the implant remains loose and will eventually need removal.
Impact on Bone Density
Long-term smoking is linked to bone loss in the jaw. For an implant to work, there must be enough dense, healthy bone to grip the post. If the bone is too thin or soft, the implant has nowhere to anchor.
Heat and Chemical Irritation
Beyond the internal effects of nicotine, the physical act of smoking creates heat and introduces toxic chemicals directly to the surgical site. This can irritate the gums, leading to inflammation and increasing the likelihood of infection.
Dry Socket Risk
If you require a tooth extraction before getting an implant, smoking creates a high risk for dry socket, a painful condition where the blood clot dislodges from the extraction site. This exposes the bone and nerves, delays healing, and complicates future implant placement.
Are Smokers Automatically Disqualified From Implants?
The Honest Answer: Not Always
Despite the risks, being a smoker does not automatically mean you cannot get dental implants. Many smokers undergo the procedure and enjoy a restored smile for years. However, it requires a different approach and a higher level of commitment.
Factors Dentists Evaluate
Your dentist will look at your specific situation rather than applying a blanket rule. Key factors include:
- Frequency: A casual smoker faces different risks than a pack-a-day smoker.
- Medical History: Do you have other conditions, like diabetes, that also affect healing?
- Bone Quality: Is there enough bone volume right now to support a post?
- Gum Health: Are there signs of active gum disease that must be treated first?
- Hygiene: How well do you take care of your existing teeth?
What Dentists Recommend Before Implant Surgery
Smoking Cessation
The single most helpful step you can take is to stop smoking. Even a temporary pause makes a difference. Quitting allows blood oxygen levels to return to normal, giving your body a fighting chance to heal the surgical site.
Recommended Timeframe
Most oral surgeons suggest stopping smoking at least one to two weeks before the surgery. Just as importantly, you should remain smoke-free for at least eight weeks after the procedure. This two-month window is when the most critical bone fusion happens. Disrupting the process during this time can be disastrous for the implant.
Adjunct Therapies
To compensate for the negative effects of smoking, your dentist might suggest additional treatments:
- Bone Grafting: Adding material to the jawbone to bulk it up before placing the implant.
- Gum Therapy: Deep cleaning to remove bacteria and improve tissue health before surgery.
- Nutritional Adjustments: Taking supplements like Vitamin C or D to support bone and tissue repair.
Also Read: Is a Full Mouth Restoration Possible With Dental Implants?
Risks Smokers Should Be Aware Of
Peri-implantitis
This is a form of gum disease that specifically attacks the area around an implant. It causes inflammation and bone loss. Smokers are much more susceptible to this infection, which is a leading cause of late-stage implant loss.
Delayed Healing
You may experience a longer recovery time. The incision sites may stay red or tender longer than they would in a non-smoker.
Greater Chance of Needing Retreatment
When an implant fails to integrate or an infection takes hold, the solution is rarely simple. Often, the failed implant must be surgically removed, and the site needs time to heal before the dentist can try again. This process resets the clock on your treatment timeline. For smokers, the cycle of placing an implant, treating complications, and potentially replacing the post means a longer road to the final result and a higher financial investment compared to patients who heal without interference.
Cosmetic Issues
Smoking contributes to gum recession. If the gums recede around the implant, the metal collar or the margin of the crown might become visible, creating a dark line near the gum.
How Dentists Improve Success Rates for Smokers
Thorough Pre-treatment Evaluation
The team performs a complete assessment. Using 3D imaging, the bone structure is mapped with high accuracy. A gum health assessment ensures that all active disease is eliminated before the surgery.
Advanced Surgical Techniques
The surgeon may use refined, minimally invasive methods to reduce trauma to the tissue and bone, which supports quicker healing.
Guided Implant Placement
We use digitally planned surgical guides. These templates help place the implant exactly where the bone quality is highest.
Laser or Ozone Therapy for Better Healing
Some practices incorporate adjunct tools like low-level laser therapy or ozone therapy. These methods are sometimes used around the surgical site to help increase localized circulation and reduce bacteria, supporting the body’s repair processes.
Strict Aftercare Protocols
Smokers are placed on frequent aftercare and hygiene schedules. These appointments help the team monitor the healing site closely and manage potential infections long before they cause significant damage.
Practical Steps to Boost Implant Success if You Smoke
Reduce or Quit Smoking
The earlier you reduce or quit, the more time your body has to restore its oxygen and nutrient delivery system, vastly improving the environment for the implant.
Maintain Meticulous Oral Hygiene
Brush twice a day and floss daily. Bacteria are the greatest threat to a healing implant, so impeccable cleanliness is paramount.
Keep Up With Professional Cleanings
Regular hygiene appointments allow the professional team to remove calcified plaque that you cannot remove at home and to keep an eye on the tissues around the implant.
Use Antimicrobial Rinses as Instructed
If your dentist prescribes a specific mouthwash, use it exactly as directed to control the bacteria in your mouth.
Follow All Post-op Instructions Carefully
Do not deviate from guidelines regarding diet, activity, and hygiene immediately following the surgery. These rules exist to protect a blood clot that forms over the incision.
Alternatives for Patients Who Cannot Quit Smoking
Sometimes, the risk profile is simply too high. If your bone density is very poor or you cannot quit smoking for the required healing period, your dentist might suggest alternatives.
- Implant-Supported Dentures: This uses fewer implants, often 2 to 4, to anchor a full denture. It is sometimes less invasive than replacing every tooth individually.
- Traditional Dentures: Modern dentures fit better than they used to. They carry zero surgical risk regarding osseointegration.
- Dental Bridges: If you still have healthy teeth on either side of a gap, a bridge can replace a missing tooth without needing surgery or bone fusion.
Also Read: Affordable Cosmetic Dentistry Options in Los Angeles: Your Options Explained
Conclusion
So, can smokers get dental implants? The answer is often yes, but it comes with conditions. Smoking undeniably increases the risks of infection and failure, but it is not always a permanent barrier.
By understanding the importance of blood flow and bone healing, and by being willing to pause or reduce smoking during the recovery phase, you significantly improve your chances.